Are you a US healthcare professional?
INDICATION
RYTELO® (imetelstat) is indicated for the treatment of adult patients with low- to intermediate-1 risk myelodysplastic syndromes (MDS) with transfusion-dependent anemia requiring 4 or more red blood cell units over 8 weeks who have not responded to or have lost response to or are ineligible for erythropoiesis-stimulating agents (ESA). See more
In second-line LR-MDS, give your eligible patients
The possibility of zero
transfusions
Study design: IMerge was a phase 3, double-blind, placebo-controlled clinical trial evaluating patients with ESA-relapsed, ESA-refractory, or ESA-ineligible LR-MDS (low or intermediate as per IPSS criteria). Patients had not received prior treatment with either an HMA or lenalidomide and were non-del(5q). Supportive care, including RBC and platelet transfusions, myeloid growth factors, and iron chelation therapy, was administered as needed per investigator discretion.1,2
RYTELO was studied in the IMerge phase 3 clinical trial1
View content
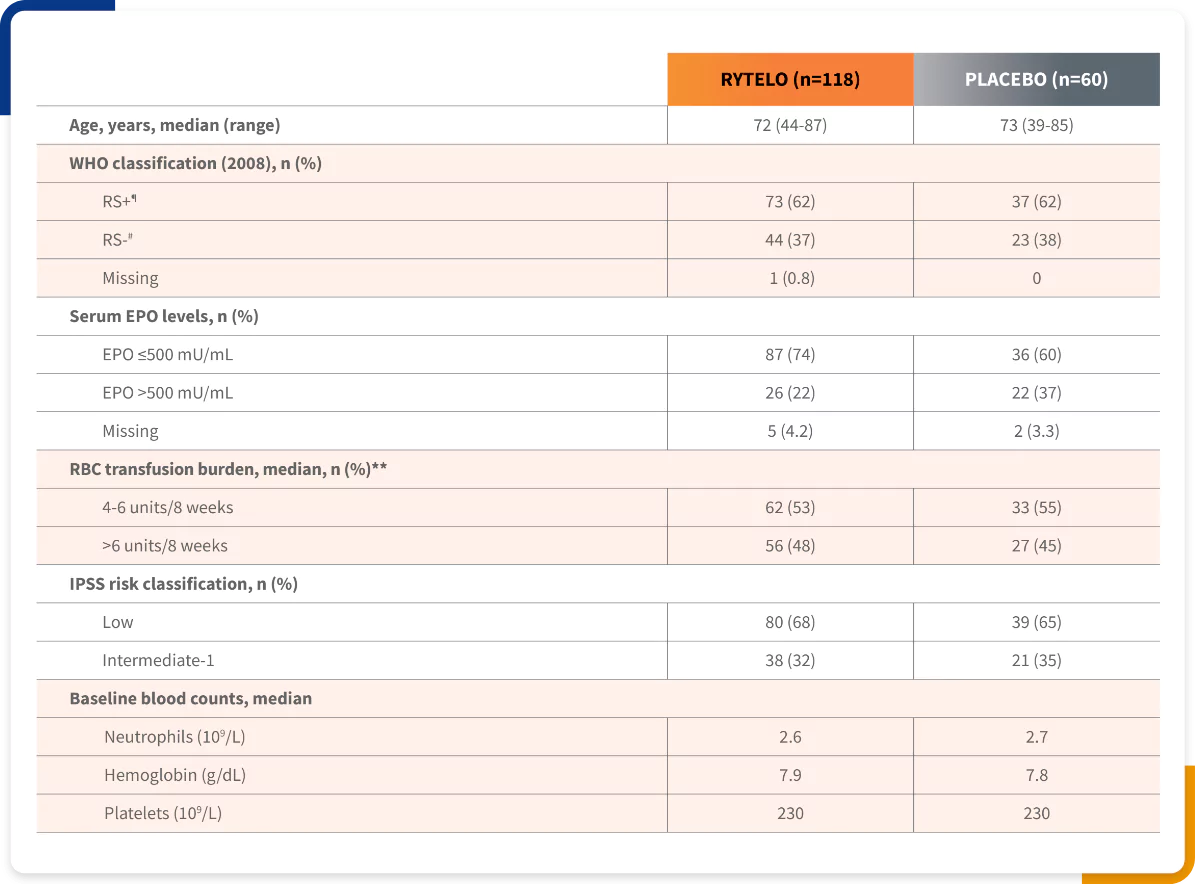
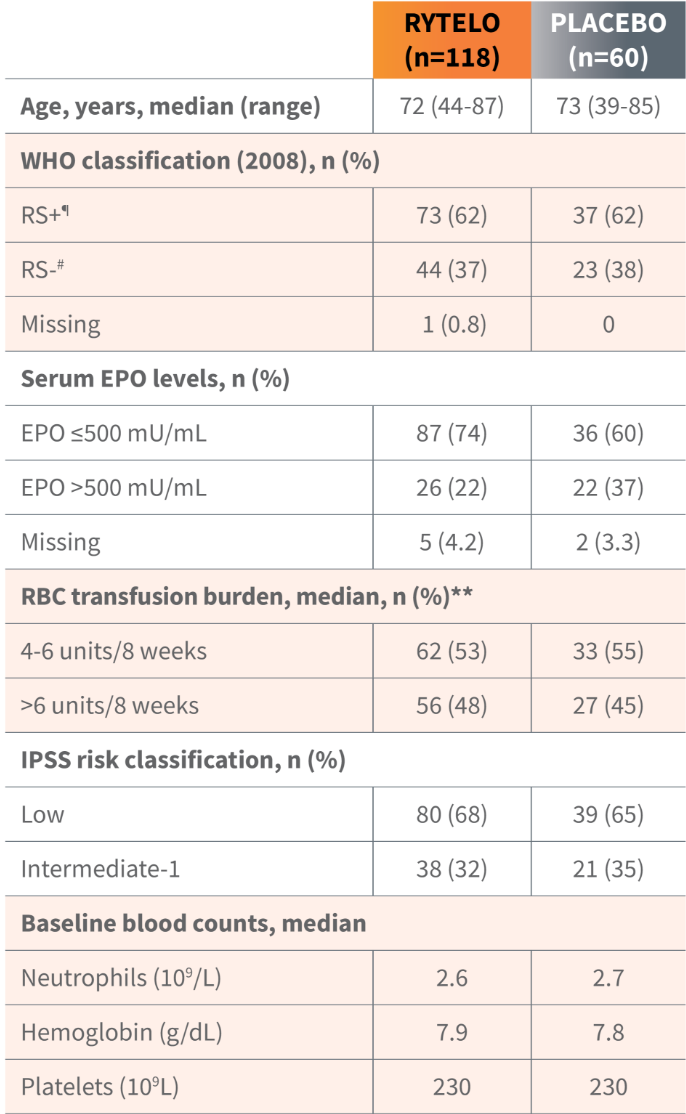
The IMerge phase 3 clinical trial assessed the safety and efficacy of RYTELO (n=118) vs placebo (n=60) in LR-MDS patients with transfusion-dependent anemia1-3
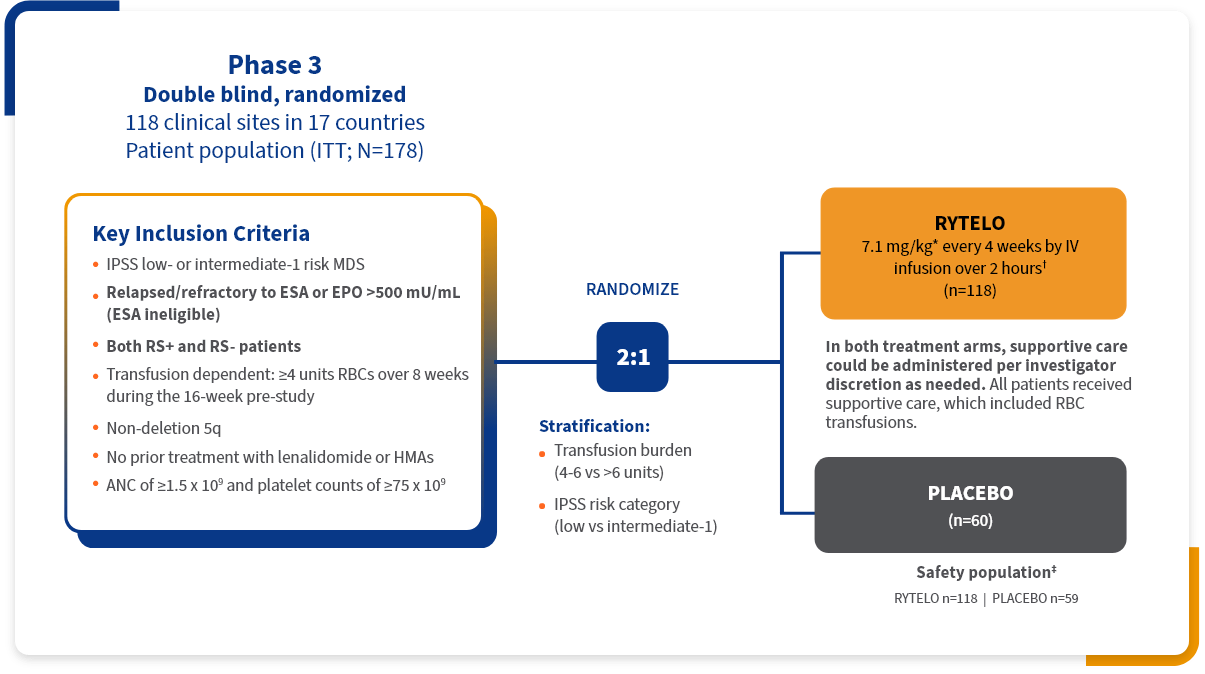
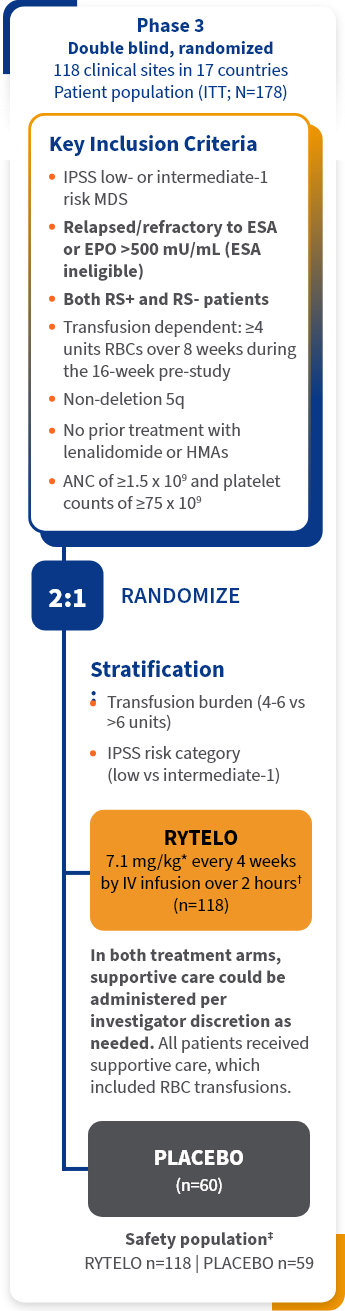
Primary endpoint:
- ≥8 consecutive weeks of RBC-TI§
Key secondary endpoints:
- ≥24 consecutive weeks of RBC-TI||
- Duration of RBC-TI
- Rate of HI-E (hematologic improvement–erythroid), measured by Hgb increase or RBC unit reduction (HI-E IWG 2006)
Key baseline patient demographics/disease characteristics1,2
Patients from the IMerge trial represented a wide spectrum of LR-MDS patients, including those with high transfusion burden, those who were ESA ineligible (EPO >500 mU/mL), as well as RS-positive and RS-negative individuals3
RYTELO provided continuous RBC-TI to patients vs placebo regardless of ring sideroblast status1
▼Limitations: This analysis was prespecified, descriptive in nature, did not control for type 1 error, and should be interpreted with caution.
Adapted from Platzbecker U and Santini V, et al. Lancet. 2024.
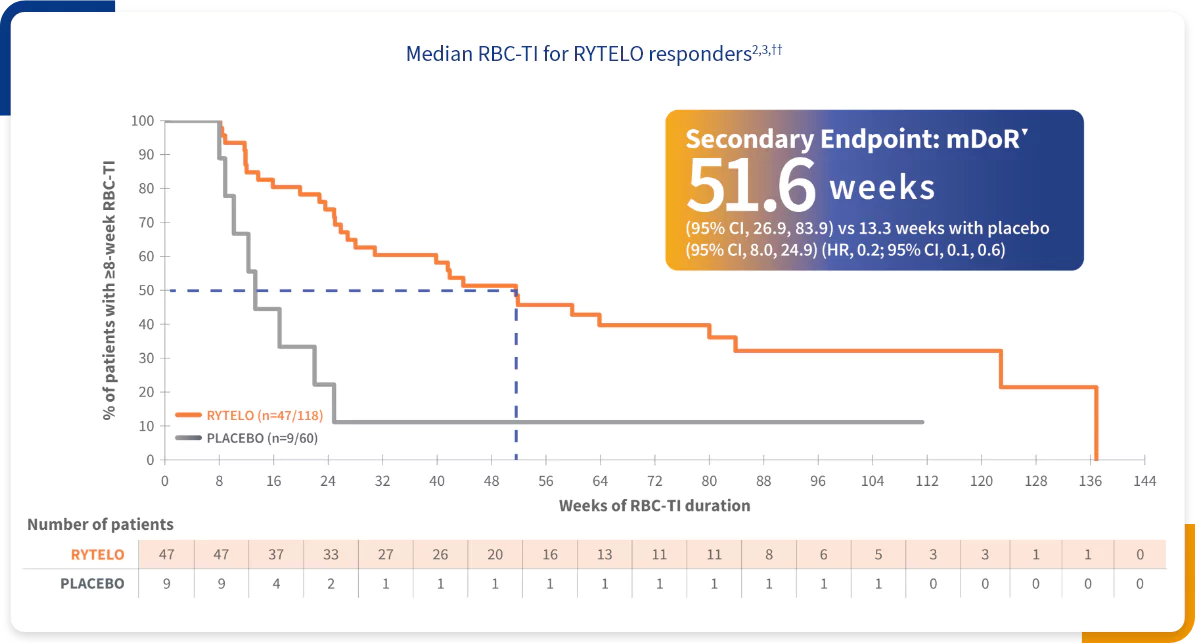
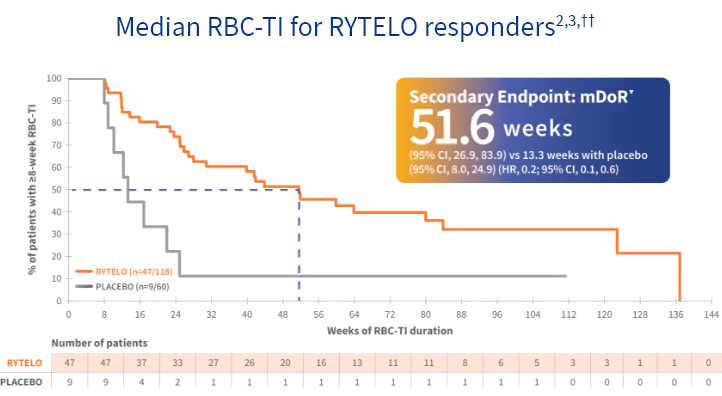
††Kaplan-Meier estimates of duration of RBC-TI; 8-week RBC-TI responder analysis set; hazard ratio is from the Cox proportional hazard model, stratified by prior RBC transfusion burden (≤6 vs >6 units RBC) and IPSS risk group (low vs intermediate-1), with treatment as the only covariate; P value for superiority of RYTELO vs placebo in hazard ratio using stratified log-rank test.2
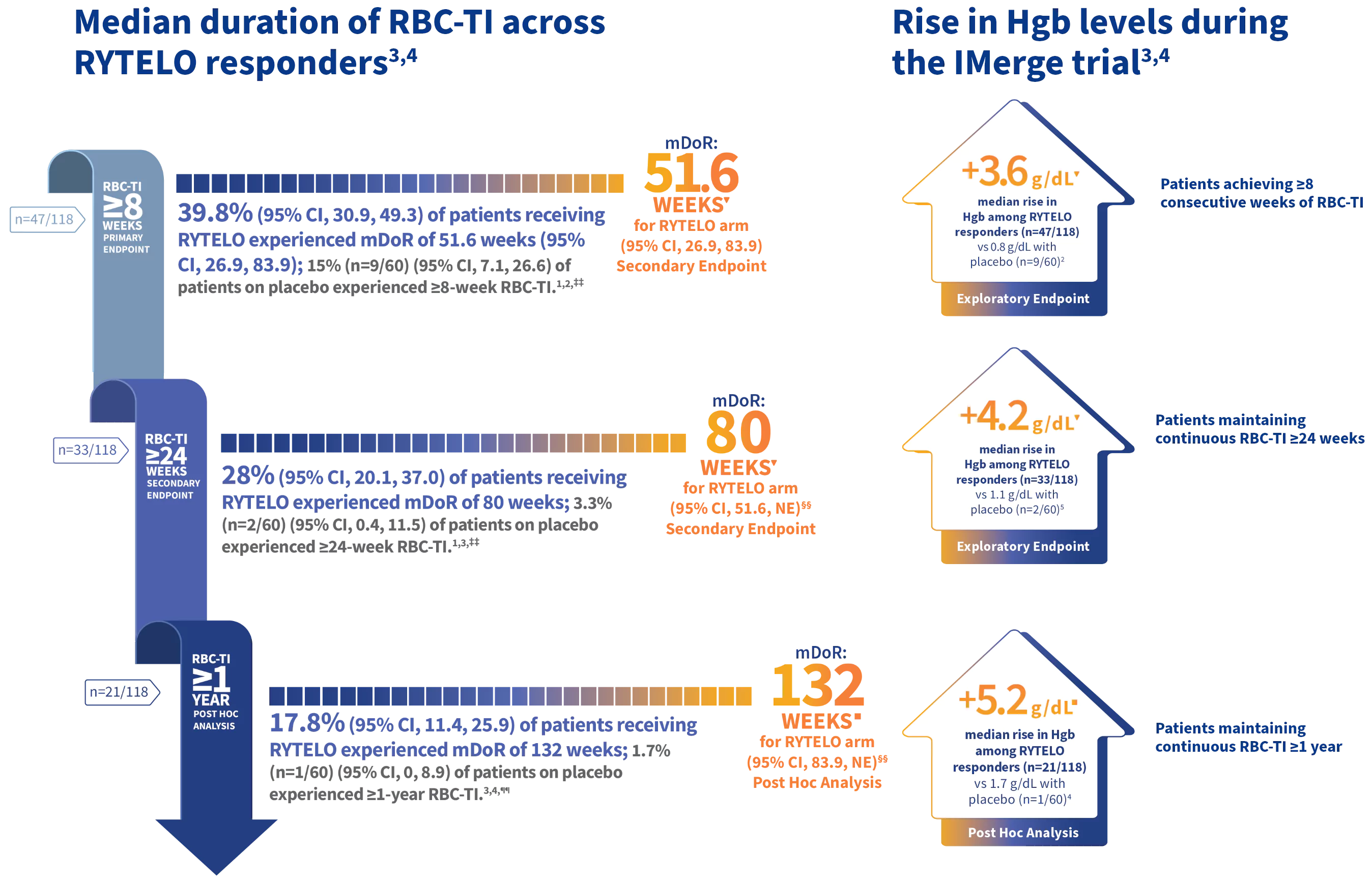
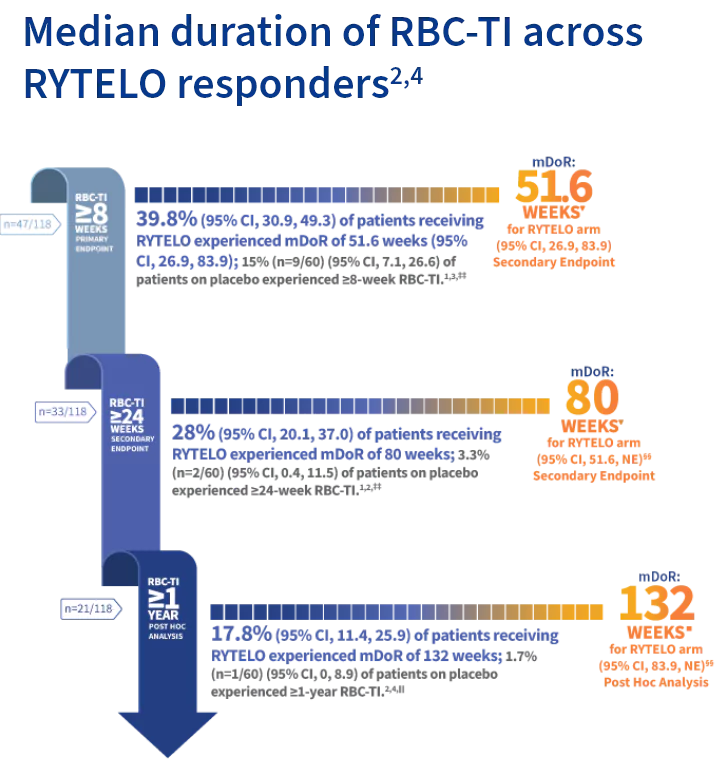

▼Limitations: These analyses were prespecified, descriptive in nature, did not control for type 1 error, and should be interpreted with caution.
■Limitations: This post hoc analysis was descriptive in nature, not prespecified, and did not control for type 1 error. Interpret with caution as results could represent chance findings.
CI based on Clopper-Pearson exact confidence interval.
‡‡≥8- and ≥24-week data cutoff: October 13, 2022.3
§§mDoR for placebo NE due to low number of responders.3
¶¶>1-year data cutoff: October 13, 2023.3
LR-MDS subgroup analyses of ≥8-week RBC-TI responders6,▼
RYTELO is the first treatment since HMAs to be FDA approved for use in ESA-relapsed/refractory LR-MDS patients without ring sideroblasts1,2,6

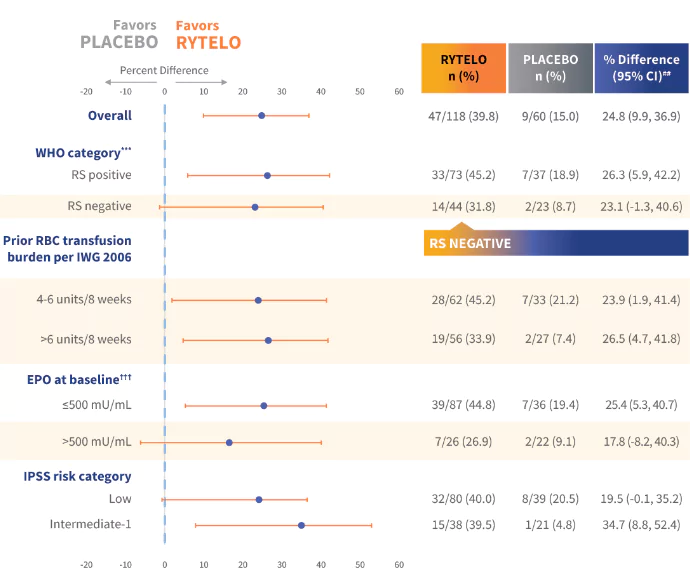
▼Limitations: These subgroup analyses were prespecified, descriptive in nature, and did not control for type 1 error. Interpret with caution as results could represent chance findings.
Adapted from Platzbecker U and Santini V, et al. Lancet. 2024.
##CI is provided for descriptive purposes only.
***One patient in RYTELO arm missing RS category.1
†††Missing data for 5 patients in RYTELO arm and 2 patients in placebo arm for the EPO at baseline category.1
ANC, absolute neutrophil count; EPO, erythropoietin; ESA, erythropoiesis-stimulating agent; Hgb, hemoglobin; HMA, hypomethylating agent; HR, hazard ratio; IPSS, International Prognostic Scoring System; ITT, intent to treat; IV, intravenous; IWG, International Working Group; LR-MDS, lower-risk myelodysplastic syndromes; mDoR, median duration of response; NE, not estimable; RBC-TI, red blood cell transfusion independence; RS, ring sideroblasts; WHO, World Health Organization.
References: 1. RYTELO. Prescribing information. Geron Corp.; 2024. 2. Platzbecker U and Santini V, et al. Imetelstat in patients with lower-risk myelodysplastic syndromes who have relapsed or are refractory to erythropoiesis-stimulating agents (IMerge): a multinational, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2024;403(10423):249-260. 3. Data on file. Geron Corporation. Foster City, CA. 4. Platzbecker U, Komrokji RS, Zeidan AM, et al. Durable continuous transfusion independence with imetelstat in IMerge phase 3 for patients with heavily transfused non-del(5q) lower-risk myelodysplastic syndromes relapsed/refractory to or ineligible for erythropoiesis-stimulating agents. Blood. 2023;142(Supplement 1):4605. 5. Zeidan AM, Santini V, Platzbecker U, et al. Efficacy of imetelstat on red blood cell (RBC)-transfusion independence (TI) in the absence of platelet transfusions or myeloid growth factors in IMerge. J Clin Oncol. 2024;42(Supplement 16):6566. 6. Platzbecker U and Santini V, et al. Imetelstat in patients with lower-risk myelodysplastic syndromes who have relapsed or are refractory to erythropoiesis-stimulating agents (IMerge): a multinational, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2024;(Supplement)403(10423):published online Dec 1. https://doi.org10.1016/S0140-6736(23)01724-5 7. Papaemmanuil E, Gerstung M, Malcovati L, et al; Chronic Myeloid Disorders Working Group of the International Cancer Genome Consortium. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood. 2013;122(22):3616-3627.
INDICATION
RYTELO® (imetelstat) is indicated for the treatment of adult patients with low- to intermediate-1 risk myelodysplastic syndromes (MDS) with transfusion-dependent anemia requiring 4 or more red blood cell units over 8 weeks who have not responded to or have lost response to or are ineligible for erythropoiesis-stimulating agents (ESA).
IMPORTANT SAFETY INFORMATION
WARNINGS AND PRECAUTIONS
Thrombocytopenia
RYTELO® can cause thrombocytopenia based on laboratory values. In the clinical trial, new or worsening Grade 3 or 4 decreased platelets occurred in 65% of patients with MDS treated with RYTELO.
Monitor patients with thrombocytopenia for bleeding. Monitor complete blood cell counts prior to initiation of RYTELO, weekly for the first two cycles, prior to each cycle thereafter, and as clinically indicated. Administer platelet transfusions as appropriate. Delay the next cycle and resume at the same or reduced dose, or discontinue as recommended.
Neutropenia
RYTELO can cause neutropenia based on laboratory values. In the clinical trial, new or worsening Grade 3 or 4 decreased neutrophils occurred in 72% of patients with MDS treated with RYTELO.
Monitor patients with Grade 3 or 4 neutropenia for infections, including sepsis. Monitor complete blood cell counts prior to initiation of RYTELO, weekly for the first two cycles, prior to each cycle thereafter, and as clinically indicated. Administer growth factors and anti-infective therapies for treatment or prophylaxis as appropriate. Delay the next cycle and resume at the same or reduced dose, or discontinue as recommended.
Infusion-Related Reactions
RYTELO can cause infusion-related reactions. In the clinical trial, infusion-related reactions occurred in 8% of patients with MDS treated with RYTELO; Grade 3 or 4 infusion-related reactions occurred in 1.7%, including hypertensive crisis (0.8%). The most common infusion-related reaction was headache (4.2%). Infusion-related reactions usually occur during or shortly after the end of the infusion.
Premedicate patients at least 30 minutes prior to infusion with diphenhydramine and hydrocortisone as recommended and monitor patients for at least one hour following the infusion as recommended. Manage symptoms of infusion-related reactions with supportive care and infusion interruptions, decrease infusion rate, or permanently discontinue as recommended.
Embryo-Fetal Toxicity
Based on animal findings, RYTELO can cause embryo-fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with RYTELO and for 1 week after the last dose.
ADVERSE REACTIONS
Serious adverse reactions occurred in 32% of patients who received RYTELO. Serious adverse reactions in >2% of patients included sepsis (4.2%), fracture (3.4%), cardiac failure (2.5%), and hemorrhage (2.5%). Fatal adverse reactions occurred in 0.8% of patients who received RYTELO, including sepsis (0.8%).
Most common adverse reactions (≥10% with a difference between arms of >5% compared to placebo), including laboratory abnormalities, were decreased platelets, decreased white blood cells, decreased neutrophils, increased AST, increased alkaline phosphatase, increased ALT, fatigue, prolonged partial thromboplastin time, arthralgia/myalgia, COVID-19 infections, and headache.
Please see full Prescribing Information, including Medication Guide.
You are encouraged to report adverse events related to Geron products by calling 1-855-437-6664 (1-855-GERON-MI) (US only). If you prefer, you may contact the US Food and Drug Administration (FDA) directly. Visit www.fda.gov/MedWatch or call 1-800-FDA-1088.
